Smart bandage measures wound healing through RFID
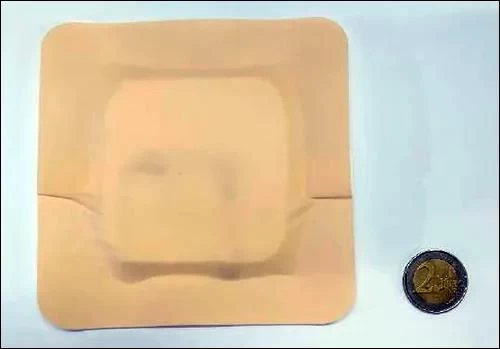
This smart bandage was developed by researchers from the University of Bologna, Italy. It is composed of humidity sensing materials, a built-in UHF RFID chip, an antenna woven in the bandage, and an off-the-shelf RFID reader that uses impedance measurement. The humidity level is determined through RFID transmission. So as to know the health status of the wound.
The research team is developing prototypes that can be 3D printed and built into commercial bandages. The researchers also tested the system using NFC technology so that users can use smartphones to wirelessly capture data without the need for a dedicated RFID reader.
Beatrice Fraboni, a professor of physics at the University of Bologna, said that in the long run, the research team hopes to cooperate with technology companies to commercialize the solution and obtain approval to start on real patients. carry out testing.
So far, Fraboni said, "The team has developed a series of bandages with different layers and different absorption characteristics", which may vary depending on the person's specific wound and healing requirements. For example, the healing process of burns and surgical incisions. The healing process of burns requires some water, and the moisture in the surgical incision may indicate the existence of potential infection.
“Our idea is that every type of wound can have its own suitable dressing,” Flaboni explained, “from slow-exuding wounds to highly-exuding wounds.” Traditional wound treatment usually requires doctors and The patient undergoes a destructive process of dismantling the wound for physical examination. The removal of the dressing from the wound usually tears the healing tissue and causes secondary damage, and this examination may also be time-consuming for the patient. They usually need to go to the doctor to examine the wound.
Therefore, the research team is committed to building a solution that includes wireless smart textiles. The bandage is made of a flexible thermoelectric material called poly(3,4-ethylenedioxythiophene) polystyrene sulfonate (PEDOT:PSS), which is screen printed on gauze and can be used to identify Changes in humidity. The RFID chip is connected to two antennas that pass through the fabric. The team’s design and engineering work involves the use of a layer of material that, once moisture is detected, can absorb and remove the liquid so that the next reading can reflect the current moisture status.
The smart bandage system monitors impedance changes based on the response to the interrogation of the RFID reader. The change in impedance depends on the dry and wet state of the antenna. The research team designed the system to adjust the settings of the reader according to the impedance to detect the appropriate sensor values to achieve the best healing according to various wounds.
Fraboni recalled that the first step in developing the system was to select materials. They wanted the materials to be biocompatible, disposable, and cheap.
And PEDOT:PSS can meet these requirements because it can be screen printed on two different types of gauze-artificial gauze and PET gauze. This material reduces potential manufacturing costs and manufacturing-related energy requirements, and is printed in the middle of the gauze in the form of a thread, while two stainless steel conductive threads are stitched on the conductive coating to be used as an RFID antenna. The RFID chip uses a unique ID number for encoding, and the reader will transmit the ID number when inquired.
Fraboni further explained that if the technology can be directly printed on gauze, it can reduce manufacturing costs and environmental impact. For example, the standard manufacturing process of depositing semiconductor chips into sensor equipment, as well as the chemicals and energy used, can all be eliminated.

In a typical application, a doctor can put a bandage on a patient's wound, and then the patient brings a leased handheld UHF RFID reader with the firmware and settings specific to the wound when the patient goes home. In this way, the corresponding threshold can be set according to the different needs of each patient, and an alarm will be sent to the doctor if the threshold is exceeded.
The patient is instructed to interrogate the RFID tag built into the bandage at specific intervals (for example, every eight hours). The data will be captured by the reader and can be displayed on the patient's device screen, and can also be transmitted to the relevant doctor via a cellular connection. The unique ID number of the bandage is associated with the patient and the impedance-based sensor readings, which can provide the doctor with information to indicate how the patient’s wound has healed.
Fraboni said that although there are already some RFID systems on the market that can detect humidity levels in specific applications, such as monitoring diapers in hospital environments and detecting leaks in automotive systems, smart bandages are designed to be more sensitive and can detect between 5 and A humidity level of 20 microliters.
Currently, researchers are working on prototypes. The plan is to build humidity impedance sensors directly into commercial bandages to provide wound healing management. It is expected that the next prototype will involve an NFC version of the bandage that can be inquired through a smartphone. Researchers hope to cooperate with technology companies to bring products to the commercial market.